Health insurance carriers and pharmacy benefit managers (PBMs) engage in “utilization review,” a process where the carrier or PBM requires that the physician or other health care practitioner submit the health care service for approval prior to the health care service being rendered under the guise of determining medical necessity. The two most common types are “prior authorization” and “step therapy". The Pharmaceutical Care Management Association argues that “[T]he major goals of prior authorization are to ensure appropriateness and suitability of the prescribed medication for the specific patient, as well as to control costs.”1 The League of Life and Health Insurers believes that “prior authorization is fundamentally care coordination. It is a layer of consumer protection that keeps them safe and also helps to control skyrocketing health care costs.”
1 Testimony submitted to the Senate Finance Committee and the House Health and Government Operations Committee dated February 15, 2023 on Senate Bill 308/House Bill 305: Health Insurance – Utilization Review – Revisions 13248_02172023_95436-396.pdf (maryland.gov)
2 Testimony provided before the House Health and Government Operations Committee on February 15, 2023 by Matthew Celentano, Executive Director.
Recent reports and articles demonstrate how these policies are abused resulting in care denials and and distracting physicians and their staff from providing care.
- The Report on the Health Care Appeals and Grievances Law for 2021 (released December 1, 2022) states that carriers rendered 81,143 adverse decisions (e.g., denials of health care services) and, for those denials appealed, the Maryland Insurance Administration modified or reversed the carrier’s decision (or the carrier reversed its own decision during the course of the Administration’s investigation) 70.5% of the time. This means that in more than 7 out of 10 cases, the Administration ruled that the carrier was wrong, and that the patient should have received the health care service.
- In 2021, the American Medical Association conducted a survey on the impact that prior authorizations have on physicians and patients and found that 93% of physicians reported delays in access to necessary care; and 82% of physicians reported that patients abandoned their recommended course of treatment because of prior authorization denials. See AMA “Fixing Prior Authorization”.
Call To Action
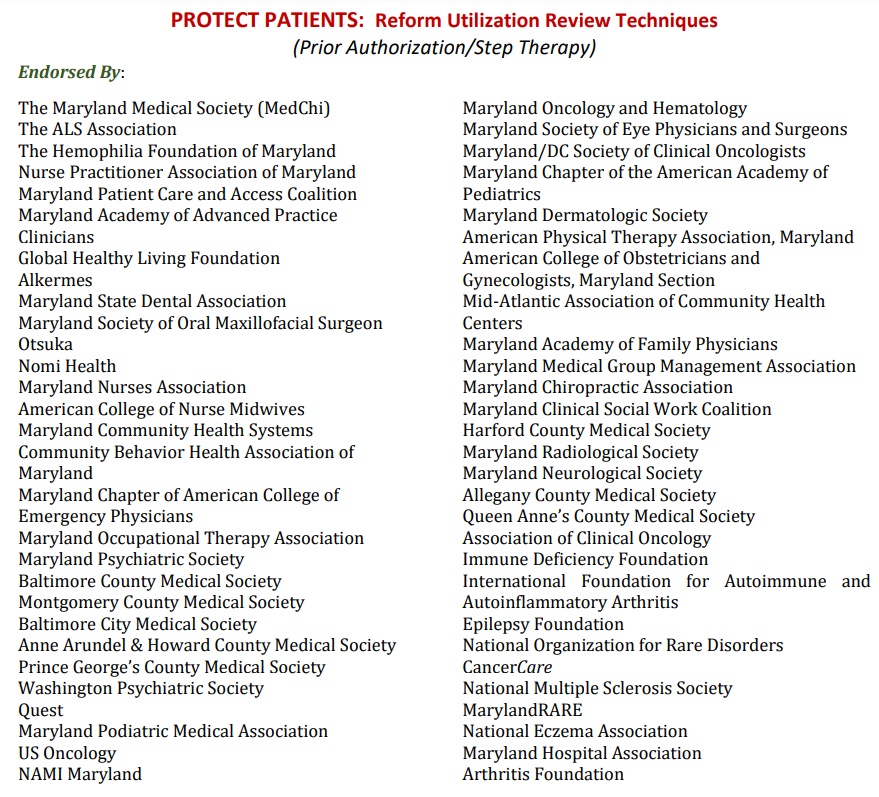
During the 2022 Session, MedChi successfully convened a coalition of over fifty organizations, representing physicians, health care practitioners, patient advocacy groups and manufacturers to support a package of reform bills on step therapy and utilization review/prior authorization. The General Assembly passed Senate Bill 515/House Bill 785: Health Insurance – Step Therapy or Fail-First Protocol and Prior Authorization – Revisions, which, beginning January 1, 2024, requires health insurance carriers to adopt a policy to approve a step therapy exception request if, based on the professional judgment of the prescriber, the step therapy drug is detrimental to the patient as specified in the legislation. After approving the step therapy exception request, the bill also states the carrier or pharmacy benefits manager (PBM) must authorize coverage for the drug rather than requiring the insured to then undergo prior authorization for the requested prescription drug. Except for an opioid that is not an opioid partial agonist, a carrier or PBM may not require more than one prior authorization if two or more tablets of different dosage strengths of the same prescription drug are (1) prescribed at the same time as part of an insured’s treatment plan and (2) manufactured by the same manufacturer. This provision addresses an issue raised by the Maryland Psychiatric Society but pertains to all medications.
The General Assembly also considered Senate Bill 308/House Bill 305: Health Insurance – Utilization Review – Revisions, which would have made comprehensive changes to the utilization review process, including prohibiting a reauthorization for a prescription drug if a patient is being well-managed on the prescription drug. While this bill did not pass, both the House Health and Government Operations Committee and the Senate Finance Committee committed to MedChi that the committees would work with the advocates over the interim to address the concerns raised by the physician community and other stakeholders in anticipation of legislation returning next Session. The Committees have requested that MedChi spearhead this effort.
Click here for a description of the organizations supporting utilization review and the legislative summaries.
Other Articles
Recent Actions by Health Plans
Despite concerns raised by physicians and patient groups, insurers continue to increase prior authorization requirements.
United Healthcare recently attempted to increase requirements on colonoscopies despite a rise in colorectal cancer. While the insurer ultimately backed down, concerns continue regarding “advance notification” for procedures.
Cigna attempted to place an additional burden on physicians, practitioners, and patients by requiring submission of office notes with all claims including evaluation and management (E/M) Current Procedural Terminology (CPT®) codes 99212, 99213, 99214, and 99215 and modifier 25 when a minor procedure is billed. Over 100 medical groups urged Cigna to reconsider this policy due to its negative impact on practice administrative costs and burdens across medical specialties and geographic regions, as well as its potential negative effect on patients. Click here to view the letter and click here to view the policy.
Ultimately, Cigna pulled back the policy and stated it was under “review.”
Have Your Voice Be Heard
Your experiences can help turn the needle in Maryland and bring change to the systems.
- MedChi has set up a dedicated email address for physicians to hear from YOU whether on past experiences or present experiences. Due to HIPPA, please remove all identifiable information.
- Has a carrier or PBM denied care, either medication or other health care service, such as a lab?
- Has a carrier or PBM required multiple drugs to be used prior to the requested drug?
- Has the process been so delayed with multiple requests for information that patient care has suffered?
- Have you requested a peer-to-peer and not been given it timely or have not spoken to a “peer”?
- Has the decision by the carrier/PBM been outside the nationally recognized standard of care?
REMEMBER – Maryland only has regulatory authority over the fully insured market and the Medicaid market. Starting in 2021, a new law requires health plans regulated by the Maryland Insurance Administration to put “MIA” on insureds’ identification cards. Medicaid managed care organizations must put “MDH” on identification cards for plans regulated by the Maryland Department of Health. The information will need to be on cards for plans issued or renewed on or after January 1, 2021 and is often located on the back of the card. However, even if you don’t see “MIA” or “MDH” but suspect that it is a fully insured market plan (e.g., small group market), send the information to MedChi. Often, plans may not have updated the ID cards.
- As a physician, you are able to submit a complaint to the Maryland Insurance Administration and ask for an expedited review when a prior authorization has been denied. MedChi can help.
Multiple complaints can trigger a market conduct examination and fine the carrier if the MIA determines that the carrier is unfairly denying care.